
Gonarthrosis is a pathological process in the cartilage tissue of the knee joint, which leads to its deformation. This process is associated with severe knee strain, wear and salt deposits.
Myths about gonarthrosis
There are 3 most famous myths:
- "The diagnosis of gonarthrosis is the prerogative of people with greater physical activity and people with a predominantly sedentary job do not suffer from it". In fact, excessive physical exertion actually contributes to the deterioration of cartilage. During sedentary work, a static effect occurs on the knees, the blood supply is prevented. In addition, a sedentary lifestyle leads to an increase in body weight.
- "Knee joint gonarthrosis is incurable, the disease progresses every day". This disease is indeed chronic, but with proper timely treatment, deterioration of the cartilage can be prevented.
- "With osteoarthritis, you have to move as little as possible and lie down more. "A patient with such a pathology is assigned special gymnastics, which strengthens the ligamentous apparatus. Only a few sports are really contraindicated.
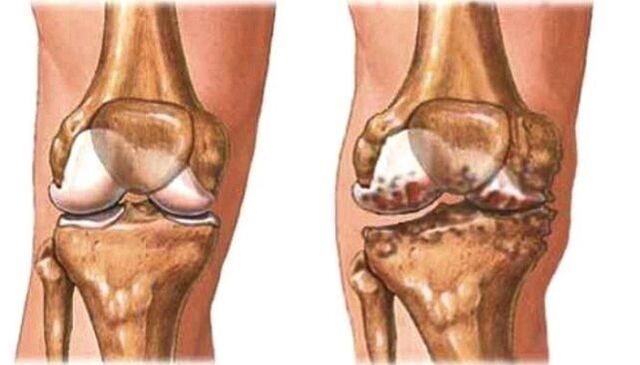
Gonarthrosis is the destruction of articular cartilage in the knee joint and adjacent bone surfaces.
Manifestations of arthrosis of the knee joint
Manifestations depend on the severity of the deformity. The more it is expressed, the more pronounced the symptoms.
Symptoms of gonarthrosis:
- long asymptomatic period;
- discomfort in the knee area;
- pain syndrome;
- reduced mobility;
- morning stiffness up to half an hour;
- the presence of a crunch during active movement;
- change of pace.
Bilateral gonarthrosis occurs when the knee joints of both limbs are involved in the process. This is one of the most serious forms. It occurs in the elderly.
Right-sided gonarthrosis is manifested by excessive static or dynamic physical exertion on the right limb. More often in athletes.
Left-sided gonarthrosis occurs in overweight people and in athletes with a load on the left leg.

The reasons for the development of gonarthrosis
Gonarthrosis is primary and secondary. Primary can occur in childhood and adolescence, which is associated with malformed joints, as well as in the elderly due to the natural aging process.
Secondary occurs due to existing injury or disease. Main reason:
- fractures, bruises, dislocations;
- excess weight;
- the presence of an inflammatory process in the joint and the lack of adequate therapy;
- metabolic diseases, which are accompanied by the deposition of salts in cartilage tissues;
- operations;
- vitamin D deficiency;
- hormonal disorders;
- weightlifting;
- some sports (running, hockey, soccer).
Who is at risk?
The risk group includes:
- professional athletes;
- obese people;
- patients who have undergone trauma or surgery;
- people over the age of 45;
- patients with varicose veins;
- those who have had cases of osteoarthritis in the family.
The risk group also includes women who wear shoes with high heels or thin, flat soles.

The exact causes of knee osteoarthritis are unknown.
The degree of gonarthrosis
Radiologically, this pathology is divided into 5 stages or degrees:
- Stage 0 - Absence of osteoarthritis on X-rays;
- Stage 1 - the appearance of a small osteophyte;
- Stage 2 - the osteophyte has clear contours, the joint space is minimally modified;
- Stage 3 - narrowing of the joint space;
- Stage 4 - pronounced narrowing of the gap, sclerosis of the subchondral bone.
Gonarthrosis of the knee 1 degree
The first degree is characterized by fatigue, limited mobility is slightly expressed, and a creak is heard. Pain appears after waking up, sitting for a long time and after physical exertion.
There are still no deformations at this stage. The x-ray shows a narrowing of the joint space.
How to treat gonarthrosis?
For treatment, a special group of drugs is used - chondroprotectors. They contain chondroitin and glucosamine, which restore the structure of the cartilage and increase its elasticity. NSAIDs are used to relieve pain.
Primary gonarthrosis is most often bilateral. Even with the development of a one-sided form of the disease, after a while the second limb is also involved in the pathological process.
The first symptoms of osteoarthritis of the knee joints are mild and unusual
Methods of treatment
In addition to drug treatment in the remission stage, the following methods are used:
- Physiotherapy;
- massages;
- leech therapy;
- ultrasound exposure;
- radon and hydrogen sulphide baths;
- phonophoresis, electrophoresis;
- paraffin compresses;
- the use of therapeutic muds.
These methods are used regardless of the stage of development of the disease during remission.
Is mud good for knee osteoarthritis? One of the indications for mud therapy are diseases of the musculoskeletal system. The course of therapy is carried out twice a year. Includes 10 to 15 procedures. The method can be used at home, and the dirt can be bought at the pharmacy.
At the first degree, the patient is prescribed orthopedic shoes for the period of exacerbation to prevent the development of the deformation process. Women are advised to wear shoes with a dense sole of at least 1 cm, a heel of 5 cm Normalize the diet - reduce the amount of salt, spicy food. Jellied meat and jelly are included in the diet, as they are natural chondroprotectors.
Another method is weight correction. Reducing body weight to an optimal level for a given patient will reduce the load on the musculoskeletal system.
Grade 2 gonarthrosis
In the second degree, the pain intensifies, as a result of which movement is significantly limited. Long-term walking for long distances causes severe pain syndrome. The patient needs to rest to continue.

If treatment is not started (or is ineffective), osteoarthritis of the knee joint progresses further.
The crunch becomes loud, lameness appears. The affected joint is deformed. An inflammatory process occurs in the inner membrane of the joint.
On simple radiography, a narrowing of the joint space, the appearance of spines on the bone (osteophytes) is found.
Treatment
Drug therapy is based on the use of NSAIDs. They have analgesic and anti-inflammatory effects. In addition, chondroprotectors are prescribed.
After the exacerbation has passed, physiotherapy exercises, massage are prescribed.
Diet recommendations:
- increase the amount of vegetables;
- include jelly and jellied meat in the diet;
- eat lean fish twice a week;
- give preference to lean meat;
- eat semolina bread.
It is also recommended to include in the diet bananas, nuts, eggs, spinach, legumes, liver, cabbage.
In addition to orthopedic shoes, special knee pads are prescribed.
Arthroscopic removal of deforming tissue is used from surgical interventions. This method has a short-term effect of 2-3 years.
Gonarthrosis of the knee, symptoms and treatment of grade 3
The most severe degree. Pain syndrome occurs during movement and at rest. Knee mobility is as limited as possible and sometimes impossible. The deformation is pronounced. There is practically no joint space on the roentgenogram.
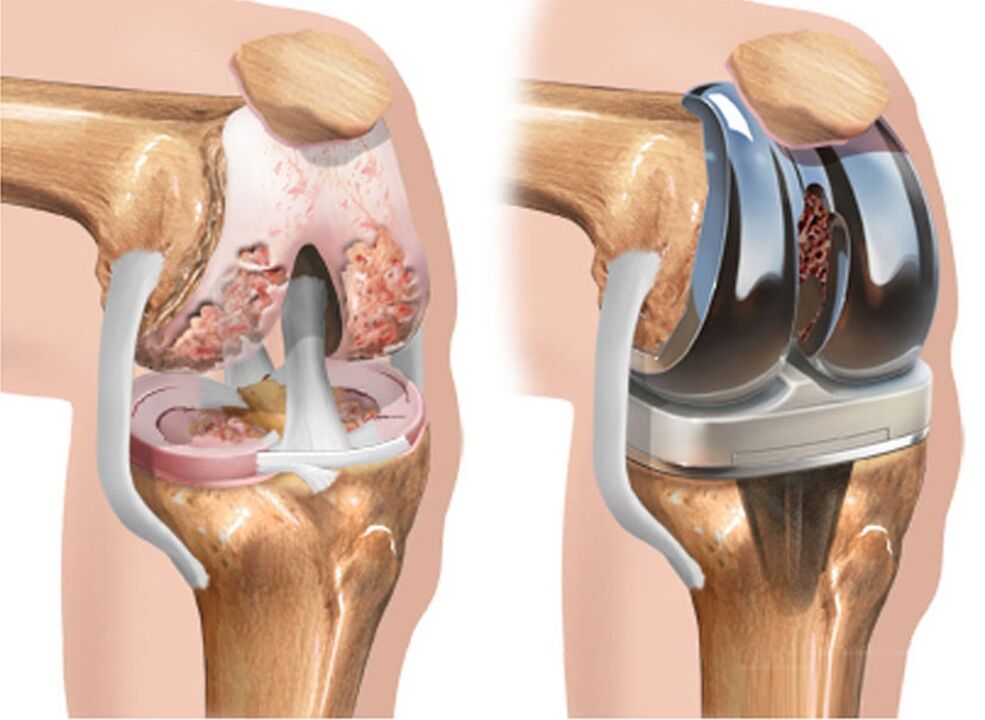
The progressive destruction of cartilage and bones in the latter stages leads to the development of ugly knee deformities, which increase in size.
Treatment
At this stage, in addition to NSAIDs, the patient is prescribed hormonal drugs. They are injected intravenously or into the joint. Severe pain syndrome is relieved by pain relievers.
In stage 3, the operation is already shown: endoprosthesis. Individual bone elements or the entire joint are replaced. Contraindication: osteoporosis.
Complications of arthroplasty:
- marginal skin necrosis;
- rejection of the prosthesis;
- neurovascular disorders (paresis, thrombosis).
In addition to the endoprosthesis, there is an arthrodesis operation - removal of deformed tissue and joint. It is rarely used.
Osteotomy - excision of the edges of the bones to redistribute the load.
Physiotherapy
Exercises for knee joint gonarthrosis can relieve pain, strengthen the muscular system and stimulate blood flow to them.
- Exercise 1. The patient lies on his back, raises his straight leg and holds it for at least 30 seconds, then the second. The running time should be increased to 2 minutes.
- Exercise number 2 "Bicycle". Lying on your back mimics cycling with your feet. Repetitions 20 to 50 times.
- Exercise number 3. The patient lies on his stomach, bends the legs alternately, trying to reach the buttocks with the heel. Repetitions 20-50 times.
- Exercise number 4. It is done the same way as the previous one, only statically. That is, the patient fixes the limb in this position for 20-30 seconds.

Patients are advised to stretch:
- Exercise 1. In a standing position, bend over, trying to reach the floor without bending the knees. Hold the position for 20 seconds, inhaling air through the nose, exhaling through the mouth.
- Exercise number 2. Sitting on the floor with his legs straight, he tries to wrap his arms around his feet, keeping his knees straight. Hold this position for up to 30 seconds. Perform 2-3 approaches. If the flexibility is not enough to reach the feet, they take the leg by the lower leg and try to pull the body as close to the legs as possible.
- Exercise number 3. The same position as when performing the previous one. The patient takes the foot by the foot, tries to straighten it and holds it as high as possible from the floor. If the exercise is difficult to perform, the leg is taken in the lower leg area. Hold the position for 10-30 seconds, then do it with the other leg.
Contraindication is the period of exacerbations and the presence of an acute inflammatory process. Patients are prohibited from running, walking for a long time and squatting.
After performing physiotherapy exercises, it is useful to massage the muscles of the thigh, lower leg on the affected limb. The joint itself should not be affected, this will increase inflammation.
Disease prevention
This disease is not hereditary, so its development can be prevented. This requires:
- avoid injuries while playing sports;
- do stretching and joint gymnastics, yoga;
- eat properly;
- maintaining a normal body weight;
- if you feel discomfort in the knee area, consult a doctor;
- drink enough water;
- after 40 years, take chondroprotective prophylaxis;
- do not overcool the joints;
- in the presence of early stages of the process and during remission, do not increase physical activity, do not rush;
- wearing orthopedic shoes;
- use knee pads when doing sports.















































